(337e) The Use of Integrated in-Vitro-in-Silico frameworks Toward De-Risking Low-Dose Dry Powder Inhalation Development
AIChE Annual Meeting
2022
2022 Annual Meeting
Pharmaceutical Discovery, Development and Manufacturing Forum
Integrated Product and Process Design with Pharmaceutical Applications I
Tuesday, November 15, 2022 - 1:54pm to 2:15pm
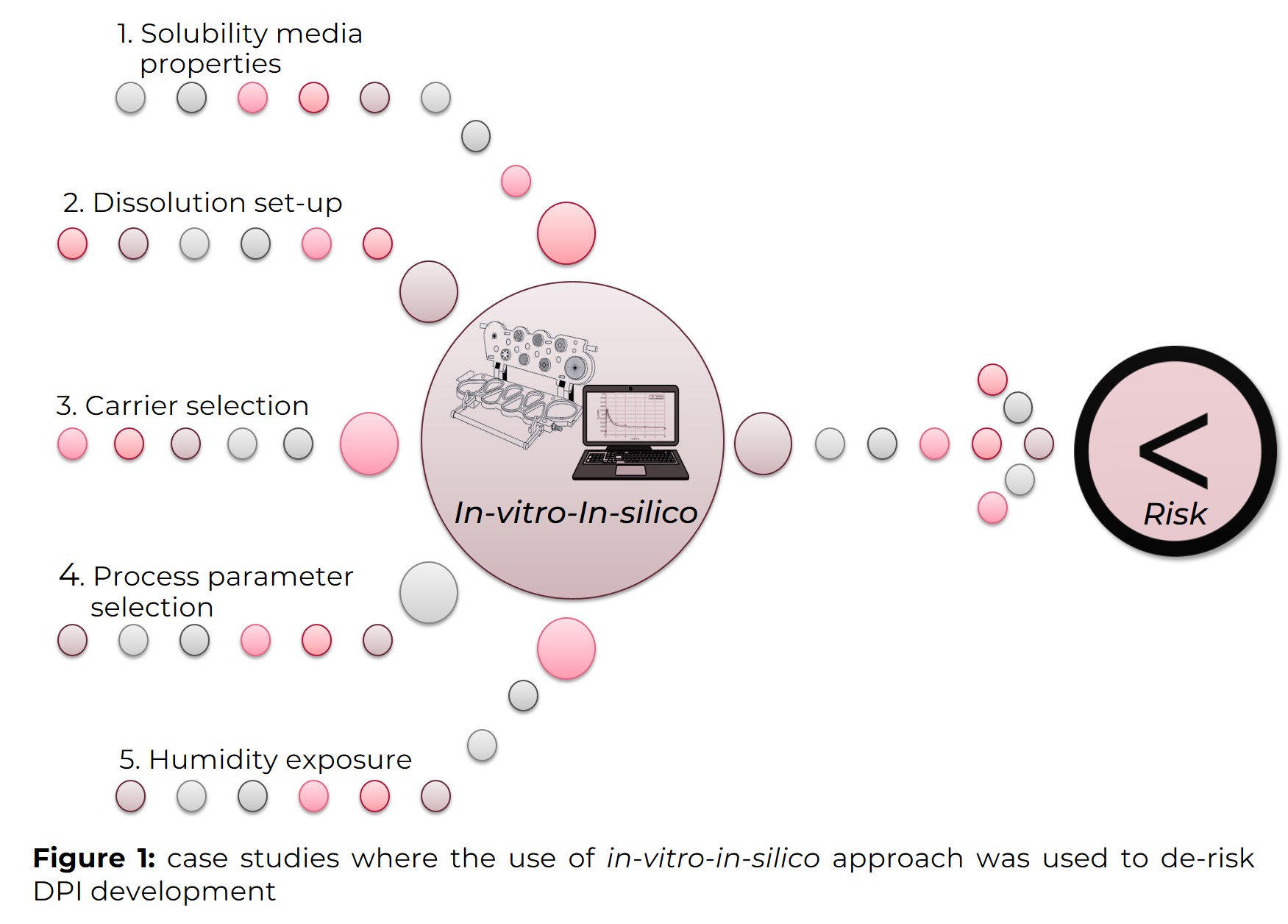
Understanding the impact that different development decisions have on the final product’s performance is vital when attempting to de-risk the drug development process. For this, it is critical to apply in-vitro and in-silico tools to predict the in-vivo performance of the developed drug. Likewise, this abstract reports a series of relevant case studies where the integrated use of distinct in-vitro and in-silico approaches has been found useful to support the development of low-dose dry powder inhalers (DPI) (Figure 1). The proposed integrated framework was used to guide the selection of bio-relevant solubility (study 1) and dissolution methodologies (study 2), help guide formulation (study 3) and process selection (study 4), and support the prediction that DPI misuse could have on therapeutic outcomes (study 5).
Materials and Methods
Different inhaled drug and carrier materials and their formulations, both in-house engineered, and commercial products were tested. For the in-house formulations, salbutamol sulphate (SS), budesonide (BUD), and formoterol fumarate (FF) were used as model active pharmaceutical ingredients (APIs) and lactose (LAC) and mannitol (MAN) as carriers. Two commercial products comprised of BUD were also tested to evaluate their in-use stability.
Solubility determination
The solubility of the different APIs was determined via the shake-flask method using distinct simulated lung fluids (SLFs) containing PBS (pH 7.4) alone or with varying combinations of albumin (protein) and lipids. An excess amount of the drugs was added to 5 mL of the media and incubated at 37°C at a shaking speed of 100 rpm for 24 h.
Adhesive mixing and blend uniformity
Adhesive mixing yielded DPI formulations containing blends of the APIs and carrier excipient particles. Mixing was performed at low and medium shear. For the low shear rate blending a Turbula blender TC2 (Willy A. Bachofen Maschinenfabrik, Muttenz, Switzerland) was applied for 90 min at 62 rpm. At medium shear, the blends were mixed in a laboratory-scale resonant acoustic mixer (LabRAM I ResonantAcoustic® Mixer, ResodynTM Acoustic Mixers, USA) for 90 s at two acceleration levels (i.e., 30 and 60 g). The blend uniformity was evaluated by measuring the content of API in 10 samples taken from different positions of the powder bed, and considered uniform at a relative standard deviation < 10%.
Evaluation of the in-vitro aerodynamic performance
The in-vitro aerodynamic performance was evaluated via next generation impactor (NGI, Copley, UK) studies. The NGI experiments were carried out with different airflows and using different inhalers. For each scenario, it was ensured that 4 L of air was drawn via the mouthpiece over the inhaler.
In-vitro evaluation of the dissolution performance
For the dissolution, the fine particle fraction was first collected using a fast screening impactor (FSI, Copley, UK). The deposited particles were ‘‘sandwiched’’ using a polycarbonate (PC) filter placed in a crystallization dish with 30 mL of medium. In sequence, the dish was put into an orbital shaker at 37°C and 60 rpm, and the dissolution was performed for 4 h, taking sample aliquots at relevant time points. An SLF containing lipids was used as the medium, and sink conditions were maintained, with respect to the solubility of the drugs.
Modeling of the in-vivo deposition
The deposition of the APIs was predicted in the Multiple-Path Particle Dosimetry v2.11 software (MPPD, Applied Research Associates, Inc). The NGI deposition profiles were used to calculate the mean mass aerodynamic geometric (MMAD) and the geometric standard deviation (GSD). In combination with spirometry profiles of the devices, the MMAD and GSD were applied to calculate the deposition of the drug in the relevant populations.
In-silico modeling of the dissolution performance
The dissolution model was developed using SimBiology® (MathWorks Inc, version R2020a). A four compartmental model describing the mass of deposited solid particles, their dissolution, permeation, and collection was built. The compartments were interconnected via the dissolution, permeation, and collection rates. The dissolution profile was predicted based on the in-vitro values obtained for API solubility and permeability and the setup details.
Physiological based pharmacokinetic modeling
Based on the available in-vivo data following their inhalation, the physiological-based pharmacokinetic (PBPK) models for the APIs were developed using GastroPlus® (Simulations Plus, USA) in its integrated PCAT (Pulmonary Compartmental Absorption and TransitTM) route module. For this, the using physicochemical properties of the API and formulations were used as inputs.
Case study results
Study 1: Influence of diverse media on APIs’ solubility and predicted in-vivo performance
Screening of the impact of different SLFs on the determination of the solubility values to be used as inputs to predict the in-vivo plasma concentration of BUD and salbutamol (SAL) showed different results depending on the nature of the molecule. For BUD, the SLF combining lipids and protein resulted in solubility values that, when used in-silico, yielded the most similar profiles to the in-vivo ones. In this medium, the solubility of BUD increased approximately five times compared to pure PBS. On the contrary, the solubility of SS remained unaffected among all investigated media; thus, no impact was observed in the predictions. This indicated that it is critical to characterize the solubility of inhaled APIs and carefully select the media for this when attempting to predict the in-vivo performance of DPIs.
Study 2: Evaluation of the use of different prediction approaches for the mean dissolution time
Successful in-vitro-in-vivo correlations (IVIVC) are dependent on the reliability of the methods used to accomplish this end. In this study, two approaches were evaluated concerning their ability to predict the mean dissolution time (MDT) and establish a level B IVIVC. The first approach used experimental values obtained in-vitro for the BUD solubility and permeability to model the dissolution in-silico. In the second approach, the MDT was deconvoluted directly from the dissolution profiles obtained in-vitro. Comparison of the in-vivo MDT of BUD to the one obtained from the in-silico model showed a prediction error of 19%. The error was notably higher (around 50%) when the MDT was directly determined from the in-vitro dissolution profile of BUD and compared to the in-vivo one. This showed that the solubility and permeability values used as input parameters for the in-silico model were adequate, however, the in-vitro dissolution methodology used was not. This indicated that further improvements were necessary to make the in-vitro dissolution set-up more bio-relevant.
Study 3: Carrier selection guidance through a PBPK framework
LAC grades presenting distinct properties were selected as model carriers and blended with a low dose of SS to be tested using a reservoir and a capsule-based device at 28, 60 and 100 L/min. The blend containing the highest fraction of excipient fines (< 10 µm) was the one that was less affected by the airflow and the one resulting in urine concentrations of SAL similar to Diskus. This showed that a certain percentage of fines (≈10%) is necessary to assure the adequate bioavailability of SS at distinct flow rates, including low ones when respiratory disease patients are unable to produce strong inhalation forces.
Study 4: Impact of adhesive blending process parameters on the predicted DPI deposition in-vivo
To evaluate the different adhesive blending process parameters’ impact on the release of the dual combination of BUD and FF formulations, the APIs were blended with an inhalable grade of MAN at different accelerations using a resonant acoustic mixer. By simulation of the deposition in-vivo, it was shown that the blending acceleration had a more notable impact on the deposition pattern of BUD when the capsule-based device was used, while, for FF more distinct impact was observed when the reservoir based inhaler was used. This set of observations underlines how a balance between the specific APIs’ particle behavior needs to be considered when defining the optimal process space for combination DPI products.
Study 5: Predicting the risk of humidity exposure on the performance of different DPI products
The use of drug-device combinations by patients is prone to errors; thus, it is essential to understand from an early stage how susceptible a formulation could be to misuse. In this study, the erroneous storage of two different commercial BUD DPIs under high humidity environments was explored. Storage of the product presenting a larger carrier particle size and a lower amount of fines resulted in less variation of the predicted AUC0-∞ values, indicating less susceptibility to high humidity storage conditions. The results of this study showed how the integration of PBPK modeling could support the late phase development of formulations less susceptible to patient misuse.
Conclusions
The series of case studies here presented, illustrate how an in-vitro-in-silico framework can be integrated from early to late phase development of low dose DPI products, de-risking development. Fit-for-purpose in-vitro analytical data can be rationally utilized in-silico at different stages of DPI product development to connect particle, formulation, and process parameters to the pharmaceutical performance.
References
Radivojev, G. Luschin-Ebengreuth, J.T. Pinto, P. Laggner, A. Cavecchi, N. Cesari, M. Cella, F. Melli, A. Paudel, and E. Fröhlich, Int. J. Pharm. 606, 120893. DOI: 10.1016/j.ijpharm.2021.120893
J.T. Pinto, I. Cachola, J.F. Pinto, and A. Paudel, Pharmaceutics 13 (3), 297. DOI: 10.3390/pharmaceutics13030297
Radivojev, J.T. Pinto, E. Fröhlich, A. Paudel, J. Drug Deliv. Sci. Technol. 52, 803-817 (2019). DOI: 10.1016/j.jddst.2019.05.047