(471e) Regeneration of the Epithelium Layer Using Fibrous Biomimetic Basement Membranes in a Mouse Dermal Wound Model
AIChE Annual Meeting
2022
2022 Annual Meeting
Topical Conference: Chemical Engineers in Medicine
Tissue Engineering, Bioprinting, and Regenerative Medicine
Wednesday, November 16, 2022 - 9:28am to 9:50am
Materials and Methods: Fiber layers (~100 μm thick) were prepared by electrospinning a 10% 99/1 wt/wt polycaprolactone (PCL)/heparin blend for 15 min. A protein mixture consisting of 10 µg/mL laminin and 20 µg/mL collagen IV was adsorbed to the fibers by incubating at 370C overnight. Scanning electron microscopy (SEM) was carried out to characterize fiber morphology and measure fiber diameters in the presence and absence of adsorbed proteins. The attachment of tracheal epithelial cells to the fibers was analyzed with a live/dead staining assay 1 and 3 days following cell seeding. Similarly, the migration of cells once in the vicinity of fibers was evaluated over a 5 day period both with qualitative staining and quantitative DNA content measurements. The presence of doses of adsorbed laminin and collagen IV proteins on fibers was characterized for its ability to induce the differentiation of basal cells to mature epithelium by establishing an air-liquid interface (ALI) culture. Gene expression of basal, mucous-secreting and ciliated cells were analyzed using NanoString® technology. Immunofluorescent staining was carried out to detect the presence of epithelium specific cell markers and SEM carried out to examine and confirm both cell presence and morphology. Next, a humanized dermal wound was developed to test the implants in mice. Here, 6 mm diameter implants were placed after creating 5 mm skin punches in the backs of mice. Wound photographs were taken every other day and the wound area measured each time. Additionally, immunofluorescent stainings to detect the presence of angiogenic and epithelial markers were carried out three weeks post-implantation.
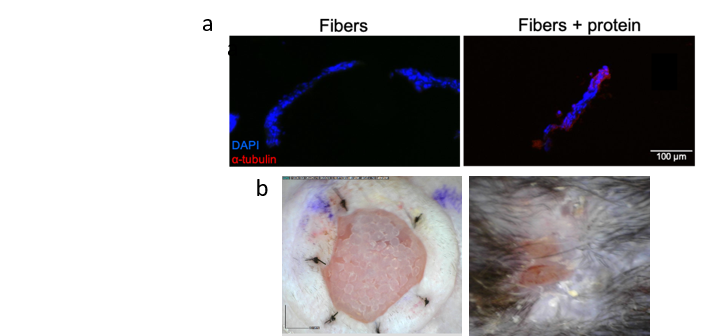
Results and Discussion: The adsorption of proteins on the fibers allows fibers to retain the same fibrillar morphology yet introduces some roughness to the fibers indicating protein deposition and the consequent appearance of larger fibers. Cell adhesion studies indicate the presence of a larger number of cells attached on fibers in the presence of adsorbed proteins. Similarly, migration studies show an increase in cell numbers migrating to fiber layers in the presence of proteins. This is vital since native basement membranes mainly act substrates for the adhesion and migration of epithelial cells. Cell differentiation experiments show that fibers enhance the expression of several mucous secreting and ciliated cell genes. Staining indicates the presence of keratin and tight cell-cell junctions characteristic to epithelial tissue while the proteins on fibers stimulate the production of ciliated cells as implied with α-tubulin staining shown in Figure 1a. This was confirmed with SEM where tight mucosal globules with protrusions and microvilli that spread across the fiber layer were detected. Wound areas decreased over the study time period and an epithelium layer was regenerated over the surface of the implants as shown in Figure 1b. Furthermore, staining studies indicated the presence of CD31, α-SMA, pan-cyto keratin and E-cadherin in the wound area further confirming healing and wound area closure.
Conclusions: The presentation of basement membrane proteins using fiber layers increases cell adherence and cell migration to fibers, stimulates the differentiation of basal cells into ciliated cells and promotes epithelialization in an in vivo dermal wound model by mimicking the composition of native membranes. Thus, the incorporation of such protein adsorbed fibers on the luminal side of tracheal replacements could ultimately facilitate the regeneration of epithelial tissue and is the current next step we are exploring.