Patients with end-stage heart failure often die waiting for a heart transplant. Today, a new engineered patch of heart muscle may extend their lives.
The engineered heart muscle patches are still in the clinical trial phase, with only 15 patients treated. But one of these patients was later given a heart transplant, allowing researchers to examine the engineered muscle graft on the patient’s original heart. Remarkably, they found that the patch was being fed by the patient’s blood supply, which supported the patient’s failing heart muscle. More importantly, that patient’s disease remained stable for the three months leading up to transplantation.
Improved solution for those awaiting heart transplants
“We now have, for the first time, a laboratory-grown biological transplant available which has the potential to stabilize and strengthen the heart muscle,” says Ingo Kutschka, the director of the department of cardiothoracic surgery at Univ. Medical Center Göttingen, who performed the surgery.
60 million people worldwide have heart failure, and 10% of those are in the advanced stage, stresses Wolfram-Hubertus Zimmerman, the director of the Institute of Pharmacology and Toxicology at Univ. Medical Center Göttingen. Sadly, 99% of patients with heart failure die without receiving a transplant.
Doctors can implant mechanical pumping devices to give patients more time in hopes of an eventual transplant, but these have high complication rates, Zimmerman adds. Researchers have long hoped to be able to shore up failing hearts with lab-grown cardiac muscle cells, but previous attempts have failed because the injected cells induced heart arrhythmias.
Muscle is grown from pluripotent stem cells
The new approach uses patches of heart muscle grown from induced pluripotent stem (iPS) cells, which are human cells — taken, in this case, from blood — that have been genetically engineered to an earlier developmental stage, enabling them to then differentiate into a variety of tissues. The researchers took these iPS cells, programmed them to differentiate into heart muscle cells and connective tissue cells, and then brought the two components together on a collagen gel. “We grow them on a mechanical training device that allows the patches to contract against load,” Zimmerman says. The result is engineered heart muscle that looks biologically equivalent to the heart muscle of a 4- to 8-year-old, he claims.
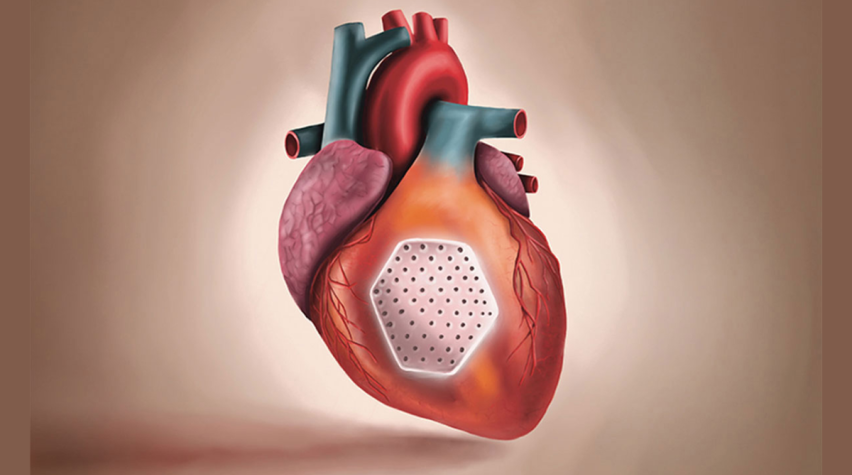
Using a 10-cm incision in the chest, the surgeon sutures a 9 cm × 4 cm patch of these cells to the beating heart. The research team initially tested the patches on rhesus macaques, experimenting with different doses of cells and various immunosuppressants.
No need to use patient’s blood as source
The cells aren’t grown from the patient’s own body. Although that might seem like a way to sidestep the risk of rejection, experiments with grafting of self-tissue in monkeys actually resulted in strong rejection, Zimmerman claims, probably because the production process of the iPS cells induces the expression of antigens on the cells, which the body then attacks. In addition, grafts with a patient’s own tissue aren’t feasible because custom-made grafts take several years to grow.
“You have to keep in mind that these patients we are treating have a mortality [rate] of 50% in 12 months,” Zimmerman states. It’s thus safer and faster to use generic iPS cells and use immunosuppressant drugs to prevent rejection.
The monkey studies revealed that the iPS cells integrated into the surrounding heart muscle and led to a thickening of the heart wall in macaques with heart failure. There were no signs of safety concerns such as arrhythmia or tumor formation.
Phase I trials underway
Zimmerman, Kutscha, and their colleagues are currently conducting Phase I clinical trials of the patches, focused on safety, dose, and side effects. They need to treat four more patients with the maximal dose of cardiac muscle cells in order to progress to a Phase II trial, which will delve deeper into patient outcomes. But they presented one case of a 46-year-old woman who received a patch in 2021. The woman had experienced a heart attack in 2016 and subsequently developed heart failure. As her heart lost the ability to pump on its own, she joined the clinical trial. Three months later, she was fortunate enough to receive a new heart. The findings provide hope that doctors can buy patients more time while they wait for a transplant.
“We always had the feeling that this was possible, but it was of course extremely important in a true clinical case we could confirm this bridge-to-transplant option,” says Zimmerman.
Clinical trials may address whether the patch is good enough to avoid the need for a heart transplant altogether, Zimmerman adds, but given how few patients ever receive a heart, the goal is to extend life for the 99% of people in end-stage heart failure who will die while on the transplant list.
“It is offering another treatment to patients that are presently under palliative care,” he says. “If we prevent heart transplantation or make it not necessary, this would be great. But we are targeting 99% of the patients, not 1%.”
Jabran, A. F., et al., “Engineered Heart Muscle Allografts for Heart Repair in Primates and Humans,” Nature, doi: 10.1038/s41586-024-08463-0 (Jan. 29, 2025).
This article originally appeared in the Update column in the March 2025 issue of CEP. Members have access online to complete issues, including a vast, searchable archive of back-issues found at www.aiche.org/cep.


