Adoptive T-cell therapy is a personalized cancer treatment that has the potential to cure previously untreatable malignancies. Researchers are applying techniques in biomolecular engineering and synthetic biology to the development of next-generation therapeutic T cells with improved safety and efficacy against a variety of cancers.
Adoptive T-cell therapy (ACT) is a new treatment that holds promise for the safe and effective treatment of cancer. Unlike traditional thera-peutics such as chemotherapy, radiation, and surgery, ACT harnesses a patient’s own immune cells as a living drug to treat previously incurable cancers.
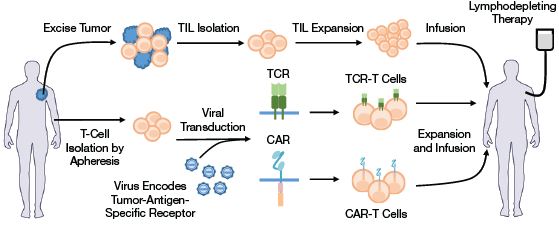
▲Figure 1. ACT uses autologous tumor-infiltrating lymphocytes (TILs) or T cells expressing a tumor-targeting T-cell receptor (TCR) or a chimeric antigen receptor (CAR). In TIL-ACT, TILs are isolated from excised tumors and subsequently expanded. In TCR/CAR-ACT, peripheral T cells are isolated from patient blood, genetically modified to express either a TCR or a CAR molecule, and subsequently expanded. Prior to T-cell reinfusion, patients typically undergo a lymphodepleting regimen (chemotherapy that depletes existing lymphocytes in the patient), which has been demonstrated to improve ACT’s treatment efficacy.
The treatment involves tumor-targeting T cells (a type of white blood cell) that are obtained by either isolating T cells that naturally target tumors or genetically modifying T cells to express a transgenic tumor-targeting receptor. These receptors could be natural T-cell receptors (TCRs) or synthetic receptors known as chimeric antigen receptors (CARs). The tumor-targeting T cells are then expanded and reinfused into the patient (Figure 1).
The leading ACT candidates are T cells that have been engineered to express CARs targeting CD19, which is a pan-B-cell marker found on the majority of cancerous B cells. In multiple clinical trials, 90% of advanced B-cell leukemia patients treated with CD19 CAR-T cells experienced complete remission (1). These results garnered immense excitement among researchers and the general public.
In July 2017, the first CD19 CAR-T cell product, CTL019 (tisagenlecleucel) from Novartis, received unanimous support from the U.S. Food and Drug Administration (FDA) Oncologic Drugs Advisory Committee for approval to treat B-cell acute lymphoblastic leukemia (B-ALL) in pediatric and young-adult patients (2). Several companies are now engaged in fierce competition to bring ACT to the market. This drive toward commercialization of ACT provides ample opportunities for chemical and biomolecular engineers to apply their expertise to the manufacturing and development of cellular products.
This article provides an overview of ACT cancer treatment and highlights the major milestones in this new therapy’s development. It identifies limitations and challenges associated with ACT, as well as strategies under consideration and developments that aim to address such challenges. Finally, it explores opportunities for engineers to make a difference in this burgeoning field.
Commercialization of ACT
In the past five years, several companies specializing in ACT as a novel cancer treatment have emerged. According to Coherent Market Insights, the global CAR-T cell market is valued at approximately $72 million in 2017 and is expected to reach $8.5 billion by 2028 (3).
Three companies at the forefront of the ACT market — Juno Therapeutics, Novartis, and Kite-Pharma — have all received “breakthrough therapy” designation by the FDA for their CD19 CAR-T cell products (4, 5). Juno Therapeutics’ JCAR015 therapy received breakthrough designation in 2014, but it experienced a major setback after several patients being treated with it died from cerebral edema (i.e., swelling of the brain) — forcing the company to terminate its clinical trial in March 2017 (6). Since then, Kite Pharma has also reported one patient death due to brain toxicity, but the company remains optimistic, while Novartis has not (yet) reported any fatalities (6). Currently, Novartis and Kite Pharma are competing to become the first to successfully commercialize their drugs, CTL019 and KTE-C19, respectively. Both Novartis and Kite Pharma expect to receive FDA approval for their drugs in 2017.
Although ACT has had substantial clinical success in the treatment of B-cell leukemia and lymphoma, significant concerns about the safety and efficacy of this novel therapy remain to be addressed. The development of new tools in biomolecular engineering and synthetic biology has enabled the engineering of T cells with safeguards against toxic and potentially deadly side effects of the treatment. In addition, T cells with better anti-tumor capabilities are being developed for the treatment of cancers beyond B-cell malignancies.
ACT: A personalized treatment for cancer
Conventional T cells play a central role in the adaptive immune system and are naturally capable of detecting and killing bacterially and virally infected cells, making them ideal candidates for cell-based immunotherapy. In ACT, the T cells’ cytotoxic capabilities are redirected against tumor cells expressing specific antigens (7). This redirection is accomplished by either naturally occurring, tumor-targeting TCRs or by transgenic receptors that are introduced into T cells via genetic engineering.
Steven A. Rosenberg and his team at the National Institutes of Health (NIH) were the first to demonstrate that cell-based immunotherapy could be used to treat cancer. They showed that the adoptive transfer of patient-derived, tumor-infiltrating lymphocytes (TILs, or T cells with innate tumor-recognition capabilities) could effectively treat patients with metastatic melanoma (8). Of the 93 melanoma patients — many with severe tumor burdens and visceral disease (characterized as stage IV cancer) — who were treated with TIL-ACT, 20 patients experienced complete regression, and 19 experienced ongoing complete regressions 3–7 years after treatment (9).
An important prerequisite for TIL-based therapy, however, is that the patient’s own immune system must contain tumor-targeting T cells that can be isolated and expanded from resected tumors. While TIL-ACT has been effective against melanoma — a uniquely immunogenic cancer where high numbers of TILs are present in the tumors — it has not been as successfully or widely applied to other types of cancer.
Engineering T cells to target cancer
To overcome limitations of TIL-ACT, scientists have engineered T cells to express transgenic receptors, which recognize tumor cells that are otherwise undetectable by the immune system (Figure 1). In this strategy, peripheral T cells are isolated from a patient and then genetically modified — using viruses that encode the genes of interest — to express receptors that recognize cancer-associated antigens. The ability to convert any T cell into an anti-tumor effector cell (i.e., lymphocytes able to eliminate tumor cells) significantly broadens the applications of ACT for the treatment of other cancers beyond melanoma.
T cells can be modified to express two types of receptors, natural and synthetic. All T cells naturally express TCRs, which recognize and bind to peptides (i.e., antigens) derived from pathogens. These pathogen-derived peptides are displayed on the cell surface by major histocompatibility complex (MHC) molecules; MHC molecules bind to the peptides and then display them on the surface for TCR recognition. All nucleated cells and platelets express MHC Class I molecules, which present fragments of cellular proteins on the cell surface. Cells infected by bacteria or viruses can present bacterial or viral protein fragments, thereby alerting T cells to the presence of infection. Tumor cells that express mutated proteins can similarly present tumor-associated protein fragments via MHC molecules, thus allowing T cells that express cognate TCRs to recognize tumor cells. The binding of TCRs to the peptide-MHC complex on tumor cells activates the T cells and triggers an anti-tumor immune response.
Scientists have identified genes that encode TCRs to target a variety of cancer antigens (9). In an early example, adoptive transfer of T cells that were genetically modified to express a TCR that targets melanoma-associated antigen 1 (MART-1) induced the regression of advanced melanoma (10). TCR-ACT has also been applied in the treatment of other epithelial cancers (9).
Despite its therapeutic potential, however, TCR-ACT still has several limitations. First, TCRs can only recognize tumor cells via peptides presented in the MHC complex. To avoid detection by TCRs, tumor cells can downregulate (i.e., reduce) their surface MHC expression, thereby rendering the TCR-ACT treatment ineffective. Furthermore, MHC exists in several different subtypes (known as human...
Would you like to access the complete CEP Article?
No problem. You just have to complete the following steps.
You have completed 0 of 2 steps.
-
Log in
You must be logged in to view this content. Log in now.
-
AIChE Membership
You must be an AIChE member to view this article. Join now.
Copyright Permissions
Would you like to reuse content from CEP Magazine? It’s easy to request permission to reuse content. Simply click here to connect instantly to licensing services, where you can choose from a list of options regarding how you would like to reuse the desired content and complete the transaction.
